Health economic evaluations have adopted an illogical parameter and the budget decision makers should be aware of it.
In the healthcare sector, we all should think and talk more about the Quality Adjusted Life Year (QALY) metric and its impact on decision making. QALY is becoming more and more common in Health Technology Assessments (HTA) and in value-based healthcare related discussions. The reason why there should be an ongoing discussion about QALY, is that it contains logical fallacy as a metric which may lead to decisions that undervalue survivability in the healthcare context.
Background
QALY is used primarily in economic evaluations to compare pharmaceutical treatments with each other. QALY multiplies life years (LY) by utility rate (“quality of life”, QOL).
Utility rate is a scale from death (0 or 0%) to 100% health
Documents and articles related to HTA usually use QALY cautiously as a parameter among other parameters and put the metric into a wider context, as they should. However, problems may arise when the outcomes are popularized or simplified for decision makers and for the wider audience.
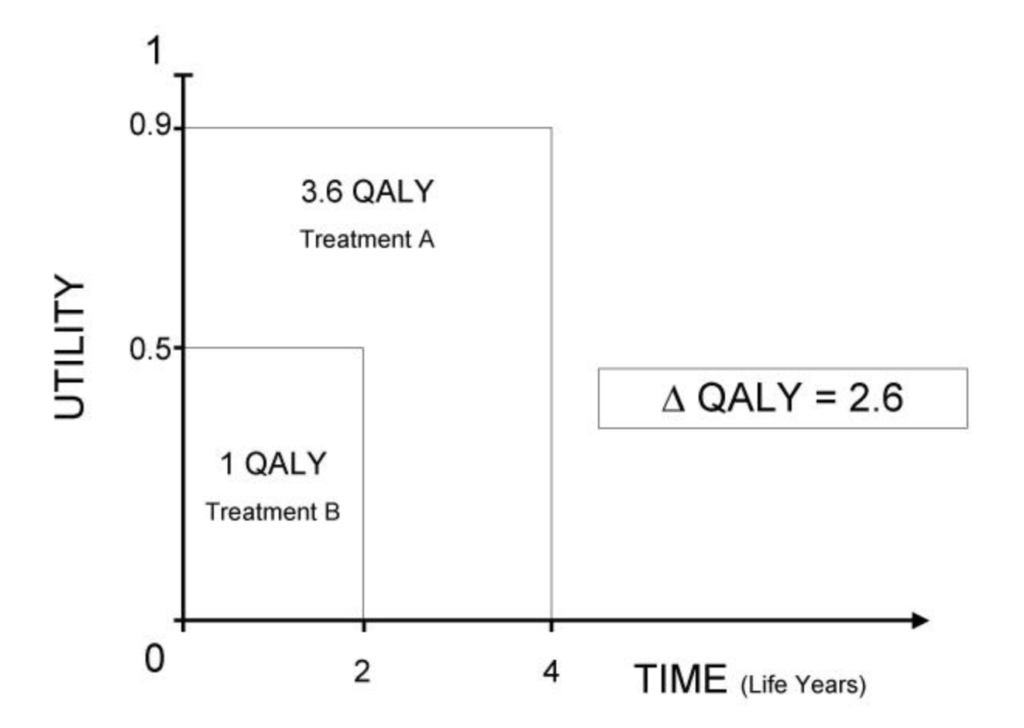
QALY is an area on the Cartesian coordinate plane: a multiplication of utility (vertical axis) and lifetime (horizontal axis).
Utility value measures people’s willingness to trade time in different health states (questionnaire survey).
The illustration below is from this article at which we will take a closer look in this post.
Why is QALY irrational?
The issue is that QALY multiplies time (years) with interval scale (quality). And as you probably know, you should not multiply continuous numbers with interval values because the outcome really tells nothing. It is the same as multiplying oranges with apples. Therefore, I made a deep dive into the dynamics of QALY as a formula and listed the observations which are good to know for all decision makers who use QALY as a part of their decision making.
Firstly, it is very unlikely that authorities approve treatments that kill (when used right). In turn, QALY as an evaluation scale starts from death. We could be a bit more practical and assume that physicians and patients are rational and stop using the drug if it does not have any impact. Medication choices are not always choices between life and death but just medication choices. Especially when comparing the pharmaceutical treatments to each other rather than trying to answer the “treat-or-not” question.
Secondly, if you compare two different treatments and both of them keep patients alive for years and years (e.g. diabetes medicines), why not just measure costs against improved quality of life? Time is relative and marginal differences in lifetime become a less significant factor in the decision making when the total expected lifetime is long for all options. QALY is linear but the decision making in healthcare is not.
Thirdly, why calculate QALY with logical fallacy when there is a mathematically logical alternative formula available as suggested by Prieto and Sacristan in their article? Now, as a metric, QALY is an “area” between the X (horizontal) and Y (vertical) axis. Prieto and Sacristan suggest a more logical alternative where QALY measures distance to origin (0) (using Pythagorean theorem and standardization).
The Cartesian Plane and the graphical representation of a Complex Number (P). As illustrated in the below picture, Prieto and Sacristan suggest that QALY could measure distance (c) to the origin (0) rather than measure “area” on the Cartesian plane (see picture above).
Below are simplified examples with traditional QALY (A) and with redefined QALY (B) for comparison
A. Simplified example of the current version of QALY
Drug A delivers 2 years with 50% utility-rate (1 QALY).
Price is 100€, meaning 100€/QALY.
0.5 utility-rate x 2 years = 1 QALY
100 € / 1 QALY = 100 €/QALY
Drug B delivers 1 year with 100% utility-rate (1 QALY).
Price is 100€, meaning 100€/QALY.
1.0 utility-rate x 1 years = 1 QALY
100 € / 1 QALY = 100 €/QALY
B. Redefined QALY which measures distance to origin (Pythagorean theorem) and is standardized as Prieto et al. presented in their paper
Drug A = 0,7906* x 2 = 1.58 QALY => 100 € / 1.58 QALY = 63.3 €/QALYDrug B = 1* x 1 = 1 QALY => 100€ /1 QALY = 100 €/QALY
*QALY standardization-factor1: and time = 1
See the difference? The traditional QALY says nothing if utility rate and expected life years are not available for the decision maker, regardless of how well you know the logic of the formula. The redefined QALY instead clearly emphasizes survivability, and the decision maker knows that the Drug A has a longer distance to the origin than the Drug B.
The redefined QALY brings at least some additional value to decision makers whereas traditional QALY always demands other context and formula components before you know whether you are investing in quality or lifetime. Priesto and Sacristan (Health Outcomes Research Unit. Eli Lilly & Co, 2003) present more strengths of their suggestion in their paper and I strongly recommend reading it.
QALY and HTA
The main weakness of the QALY is that it disregards the fact that the calculations should support decision makers in healthcare to make the decision in two different dimensions (“quality of life” and “survivability”) and not to make that decision on their behalf. In finance, Real Options Valuation has been used always without trying to multiply two different options into one.
As a budget management tool, QALY is having significant limitations and the limitations relate primarily to the differences between different patient groups and disease context which means that QALY does not necessarily help healthcare decision makers to allocate capital where it matters most for patients. Therefore, it is somewhat surprising how often national level HTA papers, related to the pharmaceuticals, try to deliver €/QALY recommendations although it is evident that the decision must be made case-by-case. Why is there such a strong drive to make QALY as a standard metric?
Originally, technology assessments were made for national decision makers but now with QALY valuations it seems that HTA is taking more and more a role as a healthcare budget management tool on an operational unit level. If the use-case for HTA is healthcare cost control (not technology evaluation as such), we should remember that hospitals have options to adopt different management systems (e.g. zero-based-budgeting) to manage costs as well as to develop procurement practices (e.g. risk-sharing agreements with vendors).
So, initiatives such as EU HTA-body HTAR will need to balance with a difficult question: is HTA a management mechanism or advisory? In the regulated pharmaceutical market, the EU has already shown its capability to procure centrally for all (COVID-19 vaccination). Centrally steered HTA and €/QALY valuation is not the same thing but leads to the situation where the buyer side widely collaborates to assess price-point. Therefore, the QALY formula is not a small thing and it really matters how it is used in decision making.
I hope this blog gives the reader some perspectives on how impractical metric QALY is and how the QALY-results may mislead the decision makers and public audience. Additionally, this blog speculated with possible consequences of the wide use of QALY in decision making.

0 Comments